Treatment
The treatment recommended by your doctor will depend on the results of your tests, the type of cancer, where the cancer is, whether it has spread, your age and your general health. Cancer of the uterus is often diagnosed early, before it has spread, and can be treated surgically. For many women, surgery will be the only treatment they need. If the cancer has spread beyond the uterus, radiotherapy, hormone treatment or chemotherapy may also be used.
Surgery
Surgery of the uterus is usually treated by an operation to remove the uterus and cervix along with both fallopian tubes and ovaries. The ovaries are usually removed as they produce oestrogen, a hormone that may cause the cancer to grow. Removing them reduces the risk of the cancer coming back.
The surgery will be performed under a general anaesthetic. The type of hysterectomy offered to you will depend on a number of factors, including your age and build, the size of your uterus, the size of the tumour, and the surgeon’s specialty and experience. If you are pre-menopausal, the removal of the ovaries will bring on menopause. If your ovaries appear normal and you don’t have any risk factors, you may be able to keep your ovaries.
Radiotherapy
Radiotherapy (also known as radiation therapy) uses x-rays to kill or damage cancer cells so they cannot multiply. The radiation is targeted at cancer sites in your body. Treatment is carefully planned to do as little harm as possible to your healthy body tissues.
Radiotherapy for cancer of the uterus is commonly used as an additional treatment after surgery to reduce the chance of the disease coming back. This is called adjuvant therapy. Alternatively, radiotherapy may be recommended as the main treatment if you are not well enough for a major operation.
There are two main ways of delivering radiotherapy: internally or externally. Some women are treated with both types of radiotherapy.
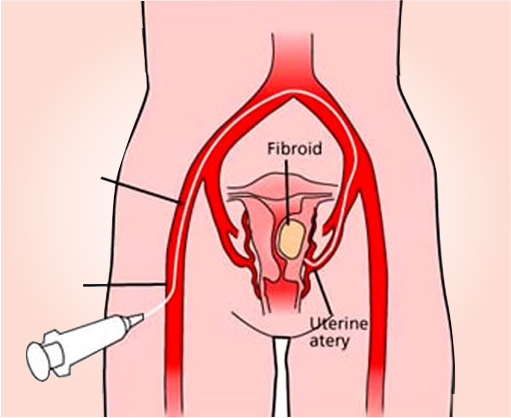
Internal radiotherapy is a way of delivering targeted radiotherapy directly to the tumour from inside your body. For cancer of the uterus, a cylinder containing radioactive material is inserted into the vagina. This cylinder is connected to a machine using plastic or metal tubes. These tubes move the radiation from the machine into your body.
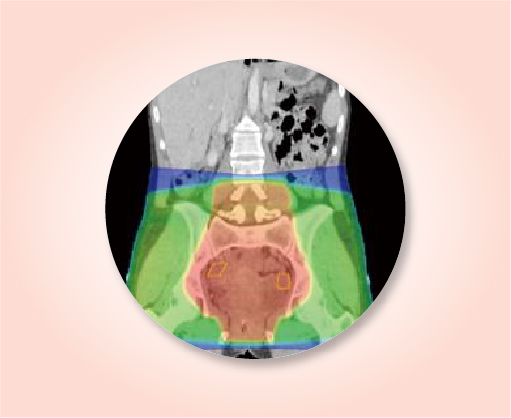
External radiotherapy directs the treatment at the cancer and surrounding tissue from outside the body. For cancer of the uterus, the lower abdominal area and pelvis are treated, but if the cancer has spread (metastasised), other areas may also be treated. You will lie on a treatment table under a machine called a linear accelerator, which delivers high energy x-rays.
You will usually have 4–5 treatment sessions, 2–3 times a week, as an outpatient. Each session will last from 5–10 minutes, but it takes much longer to set up the equipment. The applicator is taken out after each dose of radiation is delivered.
The actual treatment takes only a few minutes each time, but a lot of planning is required to make sure the treatment is right for you. This may involve a number of visits to your doctor to have more tests (e.g. blood tests) and undergo special planning scans such as a PET scan.
The machine used for external radiotherapy is large and kept in an isolated room. This can be confronting or frightening, especially when you have treatment for the first time. You may find you feel more at ease with each session you attend.
It’s very important that you attend all of your scheduled sessions to ensure you receive enough radiation to kill the cancer cells or relieve symptoms.
Hormone treatment
Hormones such as oestrogen and progesterone are substances that are produced naturally in the body. They help control the growth and activity of cells. Some cancers of the uterus depend on hormones (like oestrogen) to grow.
Hormone treatment can be given if the cancer has spread or if the cancer has come back (recurred), particularly if it is a low grade cancer. It is also sometimes offered in the first instance if surgery is not an option, for example, for young women who still want to have children. The main hormone treatment for women with oestrogen-dependent uterine cancer is progesterone.
Progesterone
Progesterone occurs naturally in women and can also be produced in a laboratory. High doses of progesterone can help shrink some cancers and control symptoms. Progesterone is available in tablet form as an injection given by your GP or nurse; or through a hormone-releasing intrauterine device (IUD) which is fitted into the uterus by your doctor

Chemotherapy
Chemotherapy uses drugs to kill or slow the growth of cancer cells. The aim is to destroy cancer cells while causing the least possible damage to healthy cells.
Chemotherapy for uterine cancer may be used for certain types:
- When cancer comes back after surgery or radiotherapy to try to control the cancer and to relieve symptoms
- If the cancer does not respond to hormone treatment
- If the cancer has spread beyond the pelvis when the cancer is first diagnosed
- In conjunction with radiotherapy.
Chemotherapy is usually given by injecting the drugs into a vein (intravenously). You may be treated as an outpatient or, very infrequently, you may need to stay in hospital overnight. You will have a number of treatments, sometimes up to six, every 3–4 weeks over several months.
Palliative treatment
Palliative treatment helps to improve people’s quality of life by alleviating symptoms of cancer without trying to cure the disease, and is best thought of as supportive care.
Many people think that palliative treatment is for people at the end of their life: however it may be beneficial for people at any stage of advanced uterine cancer. It is about living as long as possible in the most satisfying way you can.
As well as slowing the spread of cancer, palliative treatment can relieve any pain and help manage other symptoms. Treatment may include radiotherapy, chemotherapy or other medicines such as hormone treatment.
Palliative treatment is one aspect of palliative care, in which a team of health professionals aim to meet your physical, emotional, practical and spiritual needs. The team also provides support to families and carers.
