ULTRASOUND
When a suspicious site is detected in your breast through a breast self-exam or on a screening mammogram, your doctor may request an ultrasound of the breast . A breast ultrasound is a scan that uses penetrating sound waves that do not affect or damage the tissue and cannot be heard by humans. The breast tissue deflects these waves causing echoes, which a computer uses to paint a picture of what’s going on inside the breast tissue. A mass filled with liquid shows up differently than a solid mass.

Ultrasound Results : Breast Sonogram
The detailed picture generated by the ultrasound is called a “sonogram.” Ultrasounds are helpful when a lump is large enough to be easily felt, and the images can be used to further evaluate the abnormality.
A breast ultrasound can provide evidence about whether the lump is a solid mass, a cyst filled with fluid, or a combination of the two. While cysts are typically not cancerous, a solid lump may be a cancerous tumor. Healthcare professionals also use this diagnostic method to help measure the exact size and location of the lump and get a closer look at the surrounding tissue.
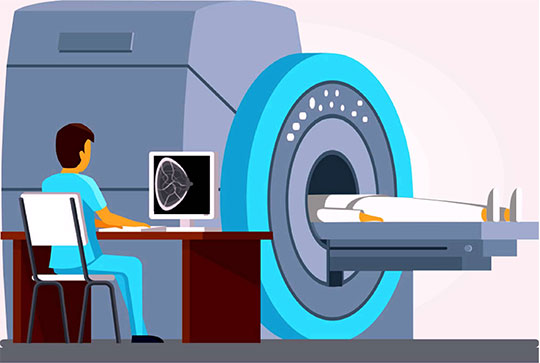
MRI ( Magnetic Resonance Imaging)
During diagnostic examinations, it is helpful to get a variety of images and perspectives. If your initial exams are not conclusive, your doctor may recommend a breast MRI (magnetic resonance imaging) to assess the extent of the disease. A MRI is more sensitive than a mammogram and an ultrasound in picking up lumps or abnormal areas in the breast. However it must be understood that all the areas picked up as abnormal by MRI are not cancer, they at time times need to be correlated with a second look ultrasound. Due to this reason MRI are used only when there is ambiguity in extent of disease or in very special circumstances.

BIOPSY
A breast biopsy is a test that removes a tiny bit of the abmormal area or lump. The removed tissue is examined under a microscope and further tested to check for the presence of cancer cells. A biopsy is the only diagnostic procedure that can definitely determine if the suspicious area is cancerous.
The good news is that 80% of women who have a breast biopsy do not have breast cancer.
There are three types of biopsies:
- Fine-needle aspiration
- Core-needle biopsy
- Surgical biopsy
The latter two are the most commonly used on the breast. There are several factors that help a doctor decide which type of biopsy to recommend. These include the appearance, size, and location of the suspicious area on the breast. Before discussing biopsy results, let’s first distinguish between the three types of biopsies.
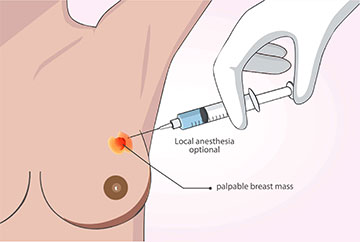
What is fine-needle aspiration?
A Fine needle aspiration cytology ( FNAC) is a method of aspirating cells with the help of a syringe and a thin needle from the tumour or the suspicious area, smearing and staining them on a glass slide and then examining them under a microscope for presence of cancer cells. FNAC are not always conclusive in their diagnosis especially when the report is negative also its difficult to distinguish a precancerous lesion from cancerous one in FNAC.
What is a core-needle biopsy?
Core needle biopsy is the procedure to remove a small amount of suspicious tissue from the breast with a larger “core” (meaning “hollow”) needle. It is usually performed under local anesthesia, meaning a small area of the breast is numbed. During the procedure, the doctor may insert a very small marker inside the breast to mark the location of the biopsy. If surgery is later required, the marker makes it easier for the surgeon to locate the abnormal area.
The radiologist or surgeon performing the core-needle biopsy may use specialized imaging equipment to guide the needle to the desired site. As with fine-needle aspiration, this may involve ultrasound.
During an ultrasound-guided core needle biopsy, the patient lies down while the doctor holds the ultrasound against the breast to direct the needle. On the other hand, during a stereotactic-guided core-needle biopsy, the doctor uses x-ray equipment and a computer to guide the needle. Typically, the patient is positioned lying on the stomach on a special table that has an opening for the breast, and the breast is compressed, similar to a mammogram.
Occasionally, no imaging equipment is used, but this is typically only in cases where the lump can be felt through the skin. This type of procedure is called a freehand core-needle biopsy.
There are fewer side effects associated with a core-needle biopsy than with surgical biopsy.
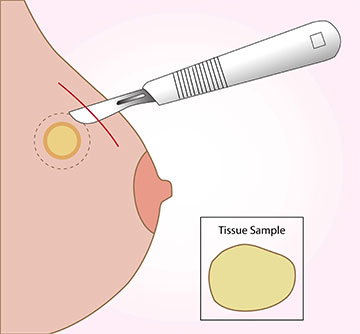
What should I expect from a surgical biopsy?
(Also known as “wide local excision”, “open biopsy” or “lumpectomy”)
A surgical biopsy can be donender local or general anaesthesia depending on the location, size of the tumour This biopsy is performed in a operation room and not in the clinic as core biopsy or FNAC.
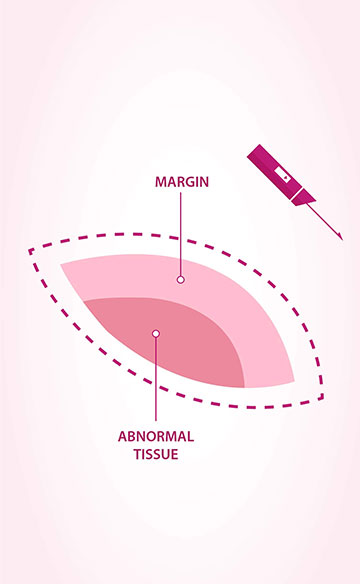
The surgeon makes an incision on skin of the breast and then removes all or part of the abnormal lump with a small amount of normal-looking tissue, known as the “margin.” If the lump cannot be easily felt but can be seen on a mammogram or ultrasound, a radiologist may insert a thin wire to mark the suspicious spot prior to the surgeon performing the biopsy. Once again, a marker is usually placed internally at the biopsy site at the conclusion of the procedure.
What do your biopsy reports say ?
Once the biopsy is complete, a specially trained doctor called a pathologist examines the tissue or fluid samples under a microscope, looking for abnormal or cancerous cells. The pathology report, which can take one or two weeks to complete, is sent to the patient’s doctor. It indicates whether the suspicious area is cancerous and provides a full picture of your situation. For the patient, waiting for results can be a real challenge, but being able to make an informed decision regarding your treatment is well worth it. Your doctor will go over the report with you and, if necessary, discuss the treatment options.
- If no cancer cells are found, the report will indicate that the cells in the lump are benign, meaning non-cancerous. However, some type of follow-up or treatment may still be needed, as recommended by the healthcare professional.
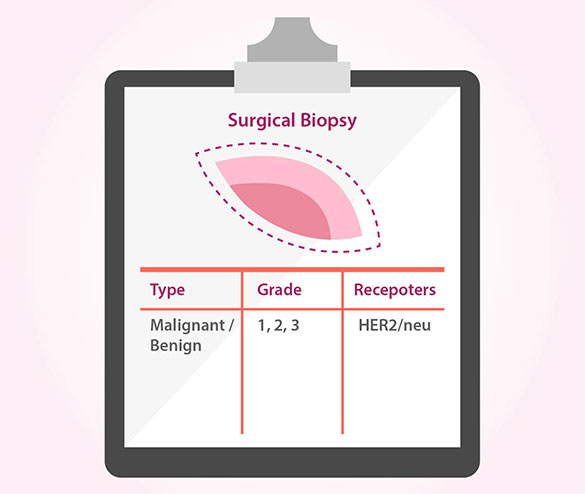
- If cancer cells are found, the report will provide more information to help determine the next steps. The report for a core-needle biopsy sample will include tumor type and the tumor’s growth rate or grade. If cancer is found, the pathologist will also perform lab tests to look at cells for estrogen or progesterone and other receptors that help in formulating a plan of treatment.
- In the case of a surgical biopsy, the results reveal data about the type, grade, and receptor status of the tumor, as well as the distance between the surrounding normal tissue and the excised tumor. The margin, as we mentioned earlier, shows whether the site is clear of cancer cells.
- A positive marginmeans cancer cells are present at the margin of the tumor. In cases of positive margins which may need to be revised surgically.
- A negative margin or clear margin indicates there are no tumor cells at the margin. That means the cancer is contained in the area nearest to the tumor.
If you are diagnosed with breast cancer, your doctor will order additional tests on the tumour to assist with treatment and prognosis. The two most common lab tests are the hormone receptor test and HER2neu test. Results from these tests can provide insight into which cancer treatment options will be most effective for you.
Testing The Tumor Cells For Hormone Receptors
A hormone receptor is a specialized protein located on the surface of or within a cell. The receptor binds to the female hormones estrogen and progesterone, which flow through the blood. Once bound, the hormone signals the cell to start growing and multiplying.
Many breast cancer tumors contain hormone receptors, often in large numbers. When hormone receptors are present, estrogen and/or progesterone can fuel the growth of the cancer. Such hormone-dependent cancers often respond well to hormone therapy, which differs from hormone replacement therapy (HRT). If estrogens receptors (ER) and progesterone receptors (PR) are absent , the cancer is said to be “hormone-receptor-negative,” and hormone therapy would be ineffective. Knowing whether the cancer cells have hormone receptors can be valuable to your medical team and your treatment plan.
Who Needs Hormone Receptor Testing?
Hormone receptor testing is generally recommended for patients who are diagnosed with invasive breast cancer,. Usually, the sample comes from a biopsy, but the test may also be performed on tissue removed during a mastectomy.
How Does The Test Work?
The testing lab typically uses a specialized staining process on the breast tissue sample to see if hormone receptors are present. The technical name for this procedure is an “immunohistochemical staining assay” or an “ImmunoHistoChemistry (IHC).” Findings will be included in a pathology report given to your doctor. If the cancer is deemed “estroge or Pregesterone-receptor-positiv” (ER/ PR+), its cells have receptors for the hormones. That means that the cancer cells likely receive signals from estrogen to promote growth. About two out of every three breast cancers are positive for hormone receptors.
If the cancer is progesterone-receptor-positive (PR+), its cells have receptors for the progesterone. This hormone could then promote the growth of the cancer.
HER2/neu Test
Similar to the hormone receptor test, the HER2/neu test looks for a specific kind of protein that is found with certain types of cancer cells and the gene that produces it. The formal name of that gene is the human epidermal growth factor receptor 2, and it makes HER2 proteins. These proteins are receptors on breast cells
In a sense, genes contain the formula for the number and combination of proteins a cell needs to remain healthy and function properly. Certain genes and the proteins they create can determine how breast cancer progresses, as well as how it responds to various types of treatment.
What is a HER2 receptor and how does it relate to breast cancer?
Healthy HER2 receptors are the proteins that help manage how a breast cell grows, divides, and repairs itself. However, in about a quarter of all breast cancer patients, the HER2 gene isn’t functioning properly. It makes an excess number of copies of itself in a process known as “HER2 gene amplification.” Then these extra genes instruct the cells to make too many HER2 receptors, which is called “HER2 protein overexpression.” The ultimate result is that breast cells grow and divide in an uncontrolled fashion.
The HER2/neu test can discover whether the sample is normal or whether it has too much of the HER2/neu protein or an excessive number of copies of its gene. If you have been diagnosed with invasive breast cancer or have had recurrent breast cancer, your doctor may recommend this test. It will help your medical team determine your prognosis, characteristics of the tumor including how aggressive the tumor is likely to be, and. Offer you targetted therapy for treatment.
This test is often ordered in conjunction with the hormone receptor test. Typically, the breast cancer tissue sample from a biopsy or the tumor removed during a mastectomy is used.
What will the HER2/neu results tell me?
There are four tests for HER2, and results of these may appear on your pathology report, which may take several weeks to come back.
The first one is the IHC test, which is short for “ImmunoHisto Chemistry.” It looks at whether there is excess HER2 protein in the cancerous cells. A result of 0 or 1+ indicates there is no excess, 2+ is borderline, and 3+ means the cells test positive for HER2 protein overexpression. Incase the report of IHC is 2 + for Her2neuoverexpression then another test is conducted on the tissue to determine the amplification of the gene. The test is called fluorescence In Situ Hybridisation or FISH. This test is able to give a response on whether or not the gene for her2neu overexpression is amplified or not
In the pathology report, breast cancers with HER2 protein overexpression and HER2 gene amplification are called HER2-positive. This type of cancer often grows faster, spreads to other areas more readily, and has a higher likelihood of recurring versus HER2-negative breast cancer.
When all three of the tests come back negative for receptors for hormones (progesterone and estrogen) and negative for HER2, triple negative breast cancer may be the diagnosis.
Blood Testing for HER2/neu
Sometimes, especially when there is not enough tumor tissue available to perform the test, a blood sample is drawn from the patient’s arm to collect similar data. This blood test is called a “serum HER2/neutest,” and it can be used as part of the initial workup upon cancer diagnosis or to monitor the effectiveness of treatment. If initially the level of serum HER2/neu is elevated to more than 15ng/mL and then it falls, the treatment is likely working. However, if the serum level remains elevated, this indicates the treatment is not working. If the serum level declines but then, upon later testing, is elevated once again, this is a sign that the cancer could be recurring.
When all three of the tests come back negative for receptors for hormones (progesterone and estrogen) and negative for HER2, triple negative breast cancer may be the diagnosis.